How much do breast implants weigh?
Saline breast implants weigh roughly 0.21 pounds per 100 cc’s, while silicone implants are slightly heavier at 0.23 pounds per 100 cc’s. Upgrading the volume of your breasts one cup size will typically require a 200 cc implant and most patients opt to add approximately 300 to 400 cc’s per breast (two cup sizes), equating to around 1.5 pounds of weight. We looked at roughly 7,000 breast implants placed in our practice over a period of ten years, and the average size was a 350 cc implant. That said, the best implant size for your cosmetic goals depends on your body frame, anatomical indicators, and desired aesthetic result.
What do breast implants feel like?
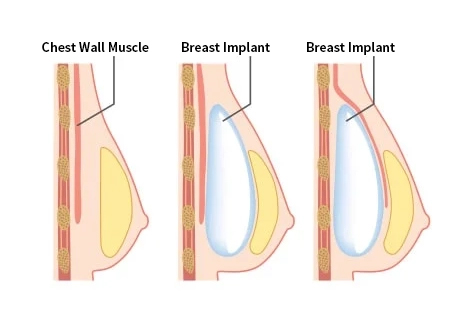
Each type of breast implant will feel differently, depending on whether saline or silicone implants are placed. Silicone implants are typically softer than saline implants, and feel more natural to the touch. No type of breast implant will feel exactly like natural breast tissue, but placing it under the muscle can decrease the likelihood of implant detection.
How should I sleep after breast augmentation?
Patients should sleep on their back while healing from breast surgery, avoiding spending long stretches of time laying on the sides or stomach for at least a few weeks.
How painful is breast augmentation?
Since breast augmentation is performed under general anesthesia, patients are unconscious and feel no pain during surgery. After the procedure, pain is manageable with oral medication and subsides within a few days. The majority of discomfort and/or tightness should dissipate within two weeks of recovery.
What type of bra should I wear after breast augmentation?
If a surgical bra is not provided, it’s generally best to wear a supportive bra that opens in the front. Sometimes our surgeons recommend an underwire bra to help shape the breast fold. A shoestring can be used in some cases to help tighten the fold. Our team will customize your individual plan because each patient is unique.
What is implant rippling and how can it be fixed?
Rippling refers to the ability to see or feel the edges of an implant underneath the skin. While this is one of the most common complications associated with breast augmentation, there are several measures that can be taken to reduce the risk of implant rippling and ensure your enhancement looks and feels natural. In certain cases, our plastic surgeon may use fat transfer to soften the edges of an implant and provide a smoother, more supple outcome. This involves taking excess fat from another part of the body and transferring it to the breast contours, thereby allowing a greater degree of coverage. If you have a petite body frame or thin breast skin, your implants may also be placed underneath the chest muscle rather than directly behind the breast tissue. This can significantly decrease the chances of rippling and give your implants more protection than an over-the-muscle approach.
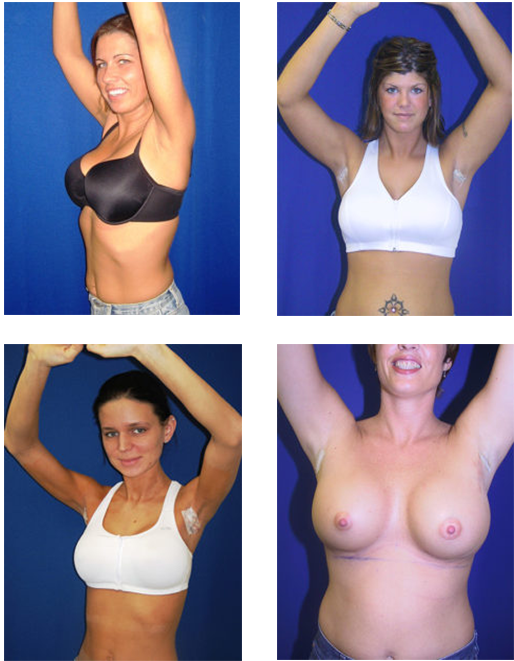
When can I exercise after breast augmentation?
It’s very important to avoid aerobic exercise and strenuous activities until you’re fully healed from your breast augmentation. The Quick Recovery® Breast Augmentation technique at our practice often allows patients to experience an accelerated recovery period when compared to more traditional approaches to the procedure. We have placed thousands of implants and typically allow our patients to exercise fully and vigorously at three weeks. This includes jogging, lifting weights, gym workouts, horseback riding, or physical intimacy. Rest assured that your plastic surgeon will give you personalized medical advice regarding when it’s safe to resume exercise after breast augmentation.
What is fat transfer breast augmentation?
Fat transfer breast augmentation, sometimes known as “natural breast augmentation,” is a technique designed to subtly enhance the breasts using a patient’s own tissue instead of implants. This approach cannot produce a significant increase in one’s breast size or breast volume, but fat transfer is often utilized to correct contour irregularities, soften the contours, and provide a very mild breast enhancement. The average size increase after two sessions of fat grafting is 170 cc, which is slightly less than one cup size. If you’re interested in lightly augmenting the breasts but prefer to avoid using implants, fat transfer breast augmentation may be an ideal treatment option. This possibility can be discussed in your consultation.
How long after breast augmentation can I swim?
As mentioned above, patients can swim three weeks after their breast augmentation procedure. Your plastic surgeon will be able to give you further insight into activity restrictions after your surgery.
Is breast augmentation safe?
Yes, the safety and predictability of breast augmentation has been extensively researched for decades and the procedure is considered very low-risk for patients who are good candidates for surgery. The best way to maximize your safety is to ensure you’re under the care of a highly experienced board-certified plastic surgeon who has a proven record of excellent breast augmentation results.
Your decision to have breast augmentation is a personal one. If the surgery has met your expectations, that’s all that matters. If you have any additional questions, or would like to schedule a consultation, please contact our practice today.